Several states have warned of another COVID wave driven by a new variant called JN.1.
The New South Wales chief health officer says the variant is partially to blame for the state’s “highest level of COVID in a year”, while Victoria’s health department says the variant has contributed to an “increase in community transmissions along with hospitalisations of COVID cases”.
However, experts say so far there has been no evidence that JN.1 is more severe.
So why is it causing more hospitalisations, and what is it doing to case numbers around Australia?
A small genetic tweak with big consequences
You can think of JN.1 as one of Omicron’s many grandchildren. It directly evolved from BA.2.86, the so-called Pirola variant that emerged in August 2023.
Back then, Pirola quickly caught the attention of scientists because it carried 30 spike protein mutations compared to its predecessor, which raised fears that it could better evade our immune systems.
Interestingly, JN.1 has just one additional spike protein mutation called L455S, but it’s a change that makes it more transmissible.
Kirby Institute virologist Stuart Turville said this particular change affected the part of the virus that binds to our cells, helping it to better evade our antibodies.
“[BA.2.86] was dominating in its own way, but it hadn’t quite navigated well past the next hurdle, which is actually navigating around antibodies,” he said.
“With JN.1, we’ve got a situation where it’s gained the competitiveness of evading antibodies like the XBBs or EG.1.”
Research published in the Lancet earlier this month found JN.1 was “significantly” more infectious than BA.2.86.
“These results suggest that JN.1 is one of the most immune-evading variants to date,” the researchers from the University of Tokyo wrote.
And while that conclusion was reached after looking at JN.1 in a lab, genomic sequencing data shows the mutation has had real-world consequences.
JN.1 has quickly become dominant in many of the countries it’s been detected in. Despite only emerging in late 2023, the variant is now responsible for more than half the COVID cases in the UK, US, France, Denmark and Singapore, according to data from the GISAID variant tracking platform.
In the US, JN.1 is estimated to make up about 62 per cent of current COVID cases, up from roughly 44 per cent just two weeks ago, the country’s Centers for Disease Control said.
How JN.1 is affecting cases in Australia
It is hard to paint a clear picture of how JN.1 is affecting cases across Australia because comprehensive COVID data has become a thing of the past.
As University of SA epidemiologist Adrian Esterman says, “it is becoming increasingly difficult in Australia to determine the current COVID situation”.
“States and territories report at different times (some monthly, some weekly, some not at all), and provide different statistics,” he said.
“The only available national collection is not up to date, difficult to use, and often provides no state/territory breakdowns.”
Some states and territories have published updates in recent weeks, indicating hospitalisations and/or cases are climbing nationwide.
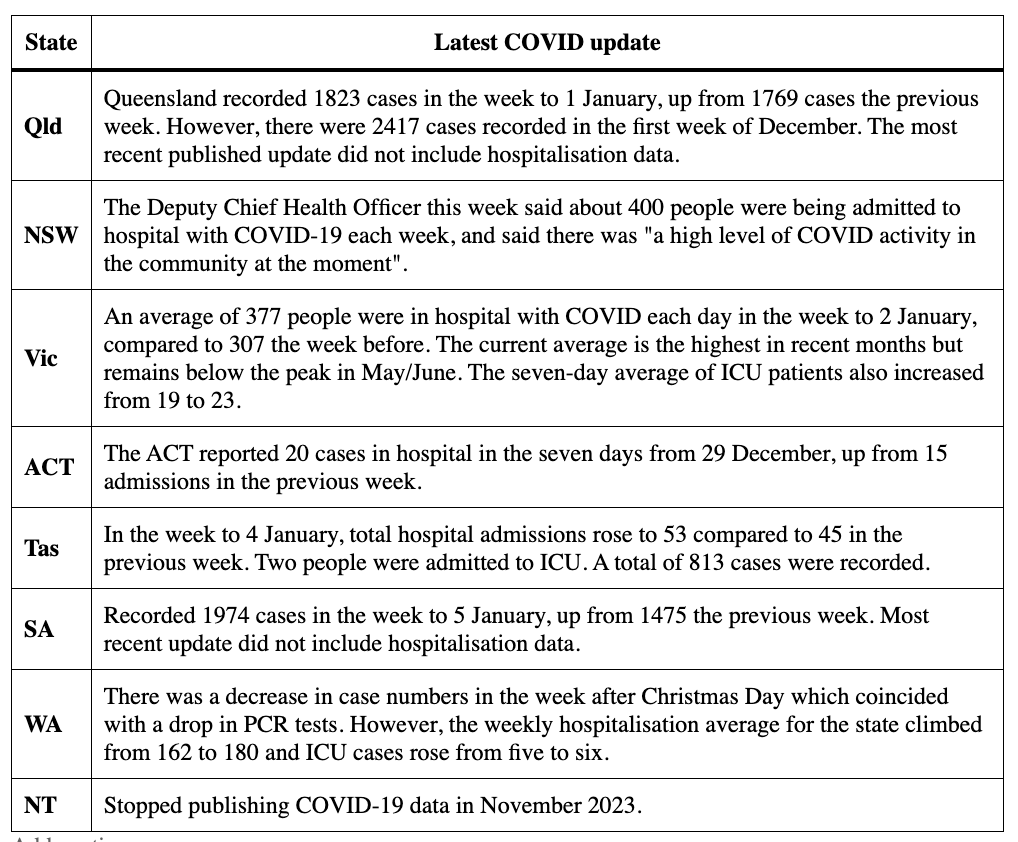
However, some states’ hospitalisation data includes people who were admitted for ailments other than COVID.
Paul Griffin, an infectious diseases physician based in Brisbane, said while Queensland was seeing a higher number of hospitalisations, the cases were on the “lower end of the severity spectrum”.
“We’re not seeing people in intensive care, and we’re seeing very low numbers of people who die from this at the moment, which is obviously a good thing,” he said.
Is JN.1 more dangerous? Not in the way you think
So JN.1 appears set to start dominating cases globally, and has been blamed for an increase in hospitalisations in Australia.
But is it more severe than other variants? So far, that hasn’t been established.
“A couple of recent studies appear to show that JN.1 has a greater affinity for lung cells than previous sub-variants of Omicron, and thus potential to cause a more serious illness,” Prof. Esterman said.
“However, in the US where 64 per cent of cases are JN.1, there does not appear to be a major increase in hospitalisations.”
Early research presented to the World Health Organization (WHO) last year also indicated that JN.1 was not more severe than other variants, although it said data was limited.
“A study from Belgium in ≥65-year-old patients has reported no difference in the odds of hospitalisation with JN.1 compared to non-BA.2.86 variants,” a WHO report published in December said.
“On the contrary, preliminary data from Singapore indicated lower risk of hospitalisation and severity in BA.2.86 elderly and younger cases.”
In its latest update, the US Centers for Disease Control said there was “no evidence that JN.1 causes more severe disease”.
So if JN.1 does not cause more severe disease, why are hospital admissions in Australia rising?
The answer comes down to simple maths.
“Increased hospitalisations over recent weeks in Australia are most likely due to more cases rather than a more severe strain,” Prof. Esterman said.
How to protect against JN.1 — and COVID in general
The usual advice for preventing COVID-19 applies: get vaccinated and stay home if you’re sick.
Six tips for staying ahead of COVID:
- Wear a mask: a high-quality and well-fitted mask can protect you and others from the virus
- Get vaccinated: stay up to date with your COVID-19 vaccine. Vaccines are available at your GP or local pharmacy
- Let fresh air in: open windows and doors when you can – it reduces the spread of the virus. Meet outside when possible
- Get tested: if you have symptoms, take a rapid antigen test. If you test positive and are eligible for antivirals, take them as soon as possible
- Stay at home: if you have COVID-19, you should stay at home for at least five days and until you have no symptoms
- Take antivirals if eligible: if you are at risk of falling very sick, you may be eligible for COVID-19 antiviral medicines.
Source: Victorian Department of Health
Experts have also highlighted that hundreds of thousands of Australians in a high risk group – being over 75 – are not up to date with vaccinations.
Data published by the federal government in December showed that only 23 per cent of people over 75 were up to date with their booster shots, and only 30 per cent of aged care residents had been vaccinated in the past six months.
“Most hospitalisations and deaths from COVID-19 in Australia are in elderly people, yet only about 20 per cent are up to date with their booster shots,” Prof. Esterman said.
“Clearly, it is this group we should be most concerned about.”
The experts have also pointed out that even though the latest COVID vaccines target a different variant, XBB.1.5, they will still help protect against serious illness and death from JN.1.
Are you up to date with your COVID vaccinations? If not, why not? Share your thoughts in the comments section below.
 © 2020 Australian Broadcasting Corporation. All rights reserved.
© 2020 Australian Broadcasting Corporation. All rights reserved.
ABC Content Disclaimer

I will not have any more Covid “vaccines” as they are a non-sterilizing vaccine and latest figures are showing an increased risk of catching it after multiple boosters. Plus an increased risk of Long Covid. Just look at the figures around the world for excess death rates, the only true measure. Way up in countries of high vaccination rates.
No thanks.