Bernardo Figueiredo, RMIT University; Catherine Itsiopoulos, RMIT University; Jacob Sheahan, The University of Edinburgh; Magdalena Plebanski, RMIT University, and Zhen Zheng, RMIT University
At least 65 million people around the world are estimated to have long COVID, which describes the continuation or development of symptoms at least three months after an initial COVID infection.
Long COVID is a complex, multi-system disease that can be disabling and may even be fatal in some cases. We still don’t understand the exact causes of long COVID, and there’s no clear treatment for it.
Over three months, we followed 14 people suffering from long COVID – or ‘long haulers’ – to better understand their experiences. In particular, we wanted to see how their ability to manage their health (called agency) and the help they get from others (social support) influence how they fare.
A few key themes
Participants recorded short videos about their daily lives, focusing on their symptoms, how they were coping, and any lifestyle changes they were making.
They experienced a range of symptoms, including fatigue, breathing difficulties and brain fog. Research has shown these are common symptoms among people with long COVID.
Participants faced psychological and social challenges, with some feeling lonely and hopeless, often made worse by social stigma around expressing mental distress. One participant said: “Most of my family haven’t contacted me that much over the last five months. So I’ve really just been on my own 24/7, which does wear anyone down.”
Another said she had not reached out to her friends too much about it because she feels like a hypochondriac.

Perfect Wave/Shutterstock
Some participants felt healthcare professionals didn’t take their experiences and symptoms seriously or didn’t understand. One described “an overall very, very poor understanding of the pathophysiology of the condition which is harming patients like me”.
Agency and social support
Although each person had a unique experience with long COVID, we were able to group these experiences into clusters based on the social support they received and the agency they had in managing their condition.
Agency is a result of multiple factors that accumulate over time including socioeconomic background, education and health literacy. Agency can improve when people feel in control of their situation.
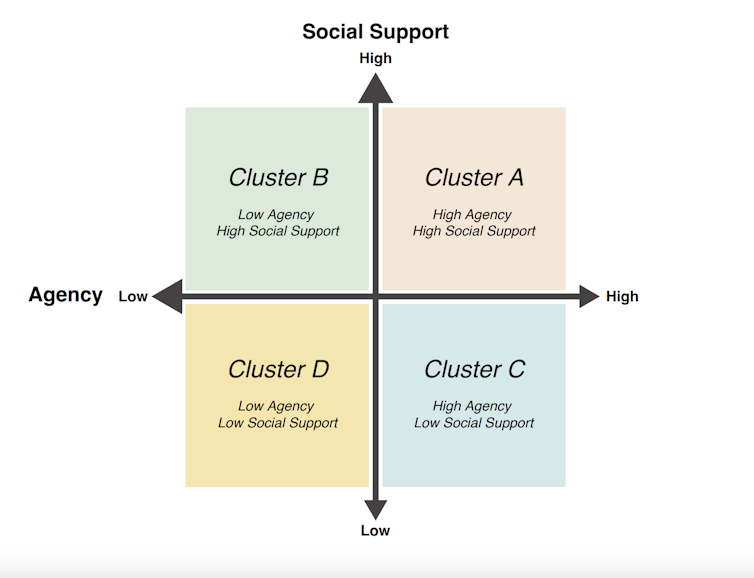
Figueiredo et al., Social Science & Medicine, 2023, CC BY
In general, those with high agency and high social support reported a better experience managing long COVID than those in the other clusters.
People with agency sought out information about their condition and potential treatments, followed through with prescribed treatment plans when available, monitored symptoms, sought support, and were involved in advocacy and research.
Social support was similarly important, manifesting in different ways – for example a spouse who helped their partner get dressed, or a manager who supported reducing work days. In some cases friends provided regular support, while family played a crucial role, often becoming long-term informal carers.
Having a wide group of supporters helped long haulers feel like less of a burden to others and avoided the fear of over-relying on an individual carer. One participant’s church group provided a helpful social network, and reinforced her self-belief. Online communities also offered support.
Those who had low agency and low social support generally reported the worst experiences. One participant who we grouped in this category said:
Long COVID has destroyed so many aspects of my life […] it’s impossible to overstate the negative impact that it’s had.
Our findings align with existing evidence
Our study was confined to a small group, and participants were only from Australia, which limits how much the findings can be generalised.
That said, our findings align with broader evidence highlighting the complexity of long COVID as a condition with both physical and psychosocial dimensions.
Our study’s emphasis on patient agency and social support also corresponds with emerging literature emphasising the important role these factors play in chronic disease management.

Josep Suria/Shutterstock
Supporting people with long COVID
We suggest healthcare professionals consider which ‘cluster’ a person with long COVID falls into (low or high agency and low or high social support) and tailor the support they offer accordingly.
For example, long haulers who are more proactive (high agency) could benefit most from educational materials suggesting, for example, different ways to cope, safe exercise routines, diet tips, and strategies to manage mental health concerns.
Meanwhile, people with long COVID who find it hard to manage their health (low agency) but have good support from others (high social support), might benefit from educational materials that show their family and friends how to help them.
Being part of online communities could also help these patients. Although online groups can provide social support and improve a person’s sense of agency, not all information shared in these communities is accurate or reliable.
And what about people with low agency and low social support?
Providing clear, straightforward information about long COVID can enhance their participation in helping manage their health.
Connecting them with support groups, communities or counselling can improve social support. Evidence shows emotional connections help reduce feelings of distress and boost wellbeing among people with long COVID.
Finally, case management services can help long haulers access and utilise community resources, and simplify their healthcare journey.
Bernardo Figueiredo, Associate Professor of Marketing, RMIT University; Catherine Itsiopoulos, Professor and Dean, School of Health and Biomedical Sciences, RMIT University; Jacob Sheahan, Research Fellow, Edinburgh College of Art, The University of Edinburgh; Magdalena Plebanski, Professor of Immunology, RMIT University, and Zhen Zheng, Associate Professor, STEM | Health and Biomedical Sciences, RMIT University
This article is republished from The Conversation under a Creative Commons licence. Read the original article.
Do you know anyone living with long COVID? How are they coping? Why not share your experience in the comments section below?
Also read: Long COVID response falls short in Australia


If people were given better advice than take paracetamol, rest and keep up your fluids, there would be far less cases of Long Covid.
Medical advice is out there if you look, but is certainly not going to come from your GP in any useful form because their hands are tied and they cannot stray from the AMA line or they risk deregistration. This is direct from my GP by the way.
Whilst I agree that people who develop Long COVID (or Post Viral Fatigue Syndrome) definitely need better medical advice, I don’t think you actually grasp the seriousness of Long COVID, Post Viral Fatigue Syndrome, or other conditions exactly like it such as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). These aren’t conditions that disappear overnight, & in the majority of cases, are never actually cured…..some people may be lucky enough to regain the majority of their health, but not all of it, while most are either home bound or bed bound…..
Any GP or doctor that says they can fix or cure anything like Long COVID or ME/CFS is worse than a quack, they’re irresponsible, despicable, & don’t deserve to call themselves a doctor.